What is - Uterine Fibroids
What are uterine fibroids?
Uterine fibroids are round and firm growths amidst the soft muscle layer of the uterus. The common name “fibroid” arises because of the pale and densely packed fibrous tissue seen when it is cut open. However, its medical term “leiomyoma” reflects its true nature as a benign (non-cancerous) growth consisting of abnormal muscle cells of the uterus rather than actual fibrous tissue.
Uterine fibroids are the most common noncancerous growths in women of any age after the onset of menstruation. The incidence increases with age. By 40 years old, more than 50 percent of women would have one or more fibroids.
What happens to uterine fibroids once developed?
Although the muscle cells made up of fibroids are abnormal in their genes, they are responsive to oestrogen, the female sex hormone.
- During the years that a woman is menstruating, oestrogen stimulation leads to the continual growth of fibroids. A fibroid increases in size by approximately 1 cm a year, but this can vary significantly depending on the individual and size of the fibroid.
- During pregnancy, fibroids are known to grow more rapidly than during the non-pregnant period. A peculiar complication of uterine fibroids during pregnancy is an uncommon change in the fibroid known as ‘red degeneration’. This condition causes abdominal pain that may require treatment with pain killers, but has no adverse outcome on the pregnancy in terms of miscarriage or premature birth of the baby.
- At menopause as oestrogen secretion ceases, many fibroids shrink in size slowly in the post-menopausal years. However, fibroids will not disappear completely, even years after menopause.
- Some other growth factors are known to influence the growth of fibroids. These growth factors are not changed by menopause. This explains why some fibroids fail to shrink or may even continue to grow despite menopause.
How are uterine fibroids classified?
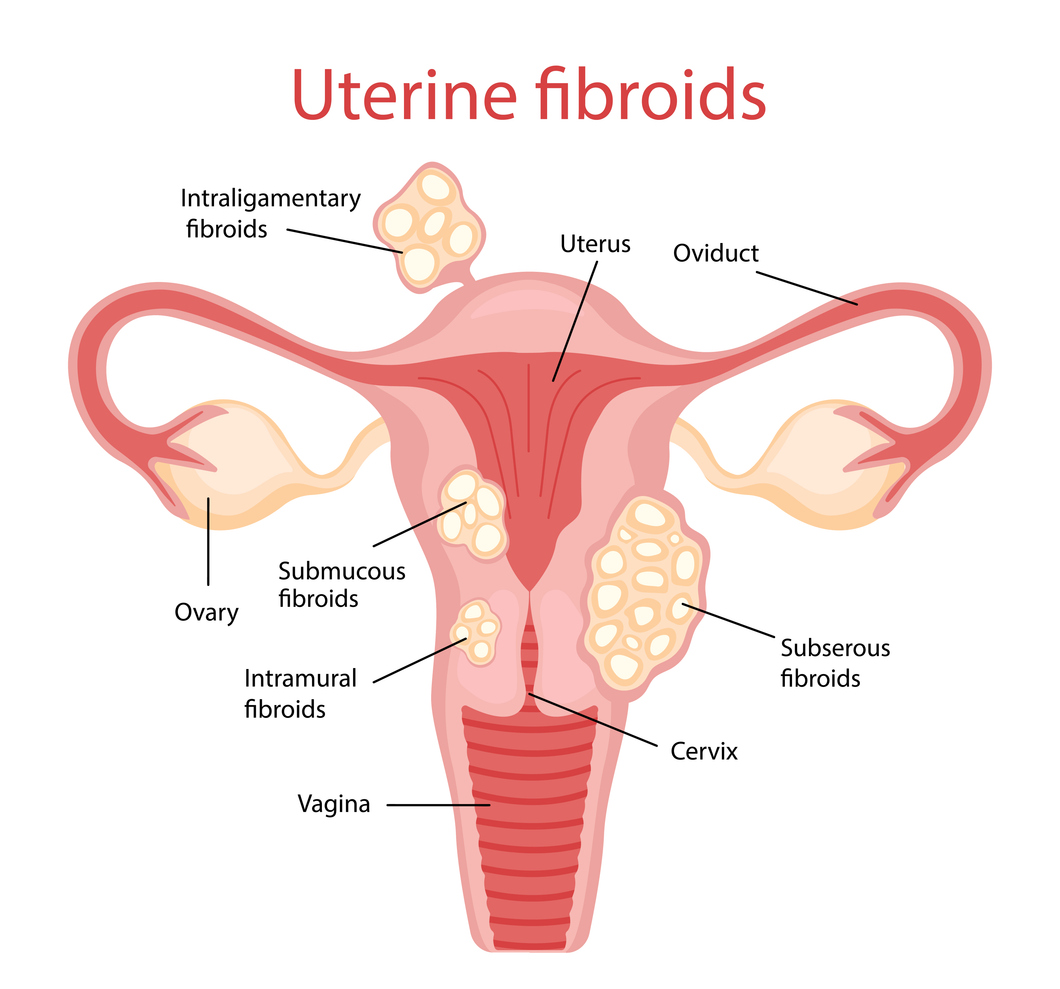
Uterine fibroids can be classified according to their size (Table 1) or by their location in the uterus (Table 2):
Table 1: Classification of fibroids by size
| Size of uterine fibroid | Category |
|---|---|
| <3 cm | Small |
| 3-5 cm | Medium |
| 6-10 cm | Large |
| >10 cm | Very large |
Table 2: Classification by location
| Location of uterine fibroid | Category |
|---|---|
Outer surface of uterus, which can cause pressure on surrounding organs |
Subserous fibroid |
Within muscle wall |
Intra-mural fibroid |
Under lining of uterus, which can cause heavy menstrual bleeding |
Submucous fibroid |
A polyp growth in the cavity of uterus |
Fibroid polyp |
Attached to the uterus by a thin stalk |
Pedunculated fibroid |
It is very common for fibroids of different sizes and locations to be present on the same uterus.
Does a uterine fibroid affect my fertility or pregnancy?
A common condition, uterine fibroids are found in many women who experience difficulty in becoming pregnant. Fibroids can impact fertility by physically obstructing the fallopian tubes, or distorting the wall of the womb and uterine lining, which can hinder sperm transport, egg implantation and overall reproductive function.
In general, most people who have fibroids go on to have an uneventful and successful pregnancy. However, depending on the location, size and type of fibroids, fibroids may increase the risk of miscarriage, preterm delivery, heavy bleeding around the time of delivery (postpartum haemorrhage), abnormal placenta location (placenta praevia), a baby that is not head-down (non-cephalic), need for caesarean delivery, and obstruction of labor if the fibroids are near the opening of the birth canal.
Symptoms of Uterine Fibroids
What are the symptoms of uterine fibroids?
Uterine fibroids are typically asymptomatic in at least 60 percent of women. They are discovered on a routine examination of the pelvis or when an ultrasound scan of the pelvis is carried out for some other reasons. In the other 40 percent of women, uterine fibroids may cause one or more of the following symptoms, depending on their size and location:
- Heavy menstrual flow
- Prolonged menstrual flow
- Symptoms and signs of anaemia from heavy menstrual flow
- Abdominal distension or pain
- Changes in urinary habits: frequent urination and sensation of not emptying the bladder completely; or difficulty in passing urine
- Constipation
- Backache
- Swollen leg from deep vein thrombosis
Uterine Fibroids - Causes and Risk Factors
What causes uterine fibroids?
Each uterine fibroid develops from a single muscle cell in which certain genes have been damaged or altered. The genetic changes lead to a more rapid cell division than usual in response to stimulation of hormones and growth factors. The cell division is also uncontrollable which results in a large number of abnormal muscle cells and the formation of a visible growth.
It is quite common for muscle cells from different parts of the uterus to develop these genetic changes over a period of time. This results in the forming of many fibroids on the same uterus.
The cause of genetic changes is currently unknown. It is clear that there is no fibroid gene that can be passed from mother to daughters in a direct genetic inheritance manner. There is also no association of fibroids with dietary habits or history of childbearing.
What are the risk factors for uterine fibroids?
The risk factors for uterine fibroids include several factors that may increase the likelihood of developing them:
- Age: Women in their 30s and 40s are more likely to develop fibroids, with the risk decreasing after menopause.
- Family history: A family history of fibroids, particularly in close relatives like a mother or sister, increases the risk.
- Ethnicity: African-Caribbean women are more likely to develop fibroids and tend to have them at younger ages compared to women of other ethnic backgrounds.
- Obesity: Being overweight or obese is linked to a higher risk of developing fibroids.
- Hormonal factors: High levels of oestrogen and progesterone, particularly during a woman’s reproductive years, can stimulate the growth of fibroids.
- Early menstruation: Women who began their menstrual periods at an early age have a slightly higher risk of developing fibroids.
Diagnosis of Uterine Fibroids
How are uterine fibroids diagnosed?
Uterine fibroids are diagnosed through a combination of medical history, physical examinations and imaging tests.

- Pelvic examination: On examination of the pelvis, a doctor may suspect a uterine fibroid if the uterus is found to be larger in size than normal or the contour of the uterus is irregular.
- Ultrasound: The diagnosis is typically based on the finding of a growth on ultrasound scan of the uterus. This is the most common imaging test used to confirm the diagnosis. It uses sound waves to create an image of the uterus, allowing the doctor to see any fibroids.
- CT Scan or MRI (Magnetic Resonance Imaging): In some cases, CT scan or magnetic resonance imaging (MRI) scan of the abdomen and pelvis will also show the presence of uterine fibroids and provide more detailed view of the size, number and location of fibroids. An MRI may also be suggested to look for atypical features of the fibroid if it is rapidly growing or very large.
- Hysteroscopy: A small telescope-like instrument is inserted through the cervix into the uterus to view fibroids inside the uterine cavity. This can either be done in the office (outpatient hysteroscopy), or in the operating theatre.
- Blood tests: Though not used to diagnose fibroids directly, blood tests may be done to check for anaemia if heavy bleeding is a symptom.
These methods help doctors accurately diagnose uterine fibroids and determine the appropriate treatment.
Treatment for Uterine Fibroids
How are uterine fibroids treated?

Most women have small or medium size fibroids. In general, these women do not experience any problem from the fibroids and do not require treatment. In other women, the decision on initiation and choice of treatment of fibroids depends on individual circumstances. The treatment available includes the following:
Treatment of heavy menstrual flow
Menstrual flow can be reduced with medication such as tranexamic acid, progesterone hormone or gonadotrophin releasing hormone analogues. This form of treatment is appropriate when the fibroid is small or medium in size. It is also more appropriate among women who are close to menopause when treatment may be limited to a short period of time before menopause ensues. This treatment is not a cure of fibroids.
Hysteroscopic resection of fibroid
Submucous fibroid or fibroid polyp can be effectively removed by resection through a hysteroscope. It is a minimally invasive procedure through the vaginal and cervical approach under general anesthesia. This technique is suitable for women of any age, including those considering pregnancy in the future. Sometimes, if the fibroid is too large, it cannot be removed within a single setting and you may be advised that you require a staged procedure – where the remaining fibroid is removed during another surgery.
Surgical removal of fibroids, also known as myomectomy
This may be recommended if you have severe symptoms like heavy menses, heavy pelvic sensation, urinary problems due to the fibroid etc.
In this operation, fibroids are removed and the uterus is repaired for resumption of its normal menstrual and childbearing functions. Fibroids of moderate to moderately large sizes can be effectively removed through laparoscopic surgery. Laparoscopic surgery involves small cuts made on the abdomen (about 1cm). Carbon dioxide is released into your abdomen to facilitate the surgery and a scope is inserted for viewing. Instruments are then placed through the small cuts to perform the surgery. The fibroids are then cut or morcellated into smaller pieces to allow removal through the small cuts. Laparoscopy is proven to be efficient and is associated with less pain and shorter recovery time compared to conventional surgery.
On the other hand, traditional open surgery, a cut of about 10-15cm on the abdomen which may be horizontal of vertical, remains the most versatile approach to remove all fibroids, regardless of the size and their location on the uterus.
Good surgical repair on the incisions on the uterus by both approaches of surgery confers additional safety on the integrity of the wounds in ensuing pregnancies. The choice of surgery depends on a few factors including the size and number of fibroids, the location of the fibroids, complexity as well as patient factors and surgeon expertise.
As with all surgeries, complications can sometimes occur even with the best effort of the surgical and nursing teams. Some of these are inherent in any operative procedure. If complications do occur, recovery may take a longer period of time and further procedures may be necessary.
What are the risks and complications of uterine fibroids surgery?
Here are some risks and complications that may occur and this list is not exhaustive:
- Common complications include bleeding and infection, wound complications (infection, breakdown, delayed healing, keloid formation), pain or numbness over the wound site.
- Other less common complications include injury to the surrounding organs (e.g. urinary bladder, bowels, blood vessels etc), formation of clots in the deep veins, scar tissue formation etc.
- In certain circumstances, if a laparoscopic surgery was planned, it may be converted to an open surgery due to technical difficulties or complications encountered.
- Even when myomectomy is successful and the fibroids are removed, new fibroids may grow.
- There is a risk of recurrence of 15-30% in 10 years.In some cases, a Caesarean section for delivery in future pregnancies will be advised if there is a concern regarding the scar on your uterus weakening and opening up during labour. Your doctor will discuss this with you after surgery.
Hysterectomy or removal of the uterus
For women who do not desire to conserve the fertility potential, removal of the uterus (hysterectomy) confers the most appropriate and complete treatment.
Uterine artery embolisation
Solitary fibroid of medium or large size can be treated by blocking the blood flow (embolisation) to the fibroid. This is an interventional radiology procedure involving inserting an arterial catheter to the uterine artery under fluoroscopic guidance. This technique is not a complete cure for fibroids.
Instead, after successful arterial embolisation, the size of the fibroid can shrink by almost 60 percent and the heavy menstrual flow can be reduced by almost 80 percent. The treatment is appropriate for women who want to avoid the risk of surgery, but some women may eventually still require surgery. It is not appropriate for women who still desire fertility whose fibroids need to be submitted for pathological tests.
Ablative therapy
Minimally invasive procedures such as radiofrequency ablation (RFA), microwave ablation (MWA) and high-intensity focused ultrasound (HIFU) have emerged in recent years. These are procedures that involve the use of heat or focused ultrasound energy to shrink or destroy fibroids. They have been shown to be effective alternative treatments for patients keen to avoid myomectomy or hysterectomy, with good fertility and pregnancy rates and short recovery times seen after treatment.
- Radiofrequency Ablation (RFA): RFA uses heat delivered through a thin device with small needles to destroy fibroids tissue. The introduction of the needle may require keyhole surgery, or surgery through the vaginal and cervix, depending on the location of the fibroid.
- Microwave Ablation (MWA): MWA uses heat generated by microwaves to destroy fibroid tissue. A probe is inserted to the fibroid guided by ultrasound, which can be done with or without incisions on the abdomen.
- High Intensity Focused Ultrasound (HIFU): HIFU uses focused ultrasound waves focused to a specific point to heat and destroy fibroid tissue. HIFU is a non-surgical procedure and no incision are required. The procedure is usually performed on an outpatient basis, often under MRI guidance.
It is important to understand that while ablative therapies can reduce fibroids size and relieve symptoms associated with fibroids, they do not remove fibroids entirely. Fibroids can still grow back and new ones can develop after treatment.
FAQs on Uterine Fibroids
Once the fibroids are removed, the uterus resumes its normal structure. There remains a 10-30 percent risk of new fibroids forming after a myomectomy. There is obviously no recurrence of fibroids if a hysterectomy is performed.
Uterine fibroids are by nature non-cancerous tumours. The malignant form of fibroid is known as leiomyosarcoma. It is a very rare tumour developed from abnormal muscle cells unrelated to fibroids. It can occur in the uterus with existing fibroids or without fibroids. Development of malignancy within an existing fibroid is extremely rare and is not a consideration for decision for surgery on fibroids.
While uterine fibroids may shrink after menopause due to the drop in oestrogen levels, they do not disappear completely. In some cases, fibroids may continue to grow despite menopause, especially if other growth factors are at play. However, if the fibroid is rapidly enlarging, there may be concerns of cancerous change and your doctor may discuss the option of surgery.
Contributed by
The information provided is not intended as medical advice. Terms of use. Information provided by SingHealth.
Condition Treated At
Department
Obstetrics & Gynaecology
Department
Obstetrics and Gynaecology (O&G) Centre
Get to know our doctors at SingHealth Hospitals in Singapore.
Get to know our doctors at SingHealth Hospitals in Singapore. here.




















