What is - Obstructive Sleep Apnoea (OSA)
What is obstructive sleep apnoea (OSA)?
Obstructive sleep apnoea is a condition where a person experiences repeated blockage to breathing during sleep. In OSA, the upper airway collapses repeatedly during sleep. This creates an effect similar to that of being repeatedly choked throughout the night.

During these episodes, sleep is interrupted and there are recurrent dips in the blood oxygen levels, putting stress on the heart. As a result, sleep is unrefreshing and you would typically feel sleepy and irritable throughout the day.
How common is obstructive sleep apnoea (OSA)?
Obstructive Sleep Apnoea (OSA) is common and a worsening global health problem. Recent data from the Singapore Health Study estimated that 30.5 percent of Singapore’s population has moderate to severe OSA. As obesity is a risk factor for OSA, the prevalence of OSA is likely to rise further in the face of the worsening obesity epidemic.
What are some complications from obstructive sleep apnoea (OSA)?
In addition to causing sleep disruption and daytime symptoms, OSA can increase the risks of serious health complications such as:
- Memory loss
- Stroke (Almost 70% of people who have had a stroke have OSA)
- Hypertension (>35% of people with sleep apnoea suffer from hypertension)
- Diabetes
- Depression
- Heart failure and heart attacks (by 2 to 3 times)
- Risk of motor vehicle accidents (by 7 times)
- Increased risk of work-related accidents
Symptoms of Obstructive Sleep Apnoea (OSA)
What are the symptoms of obstructive sleep apnoea (OSA)?
One of the most common signs of obstructive sleep apnoea is snoring or gasping for air during sleep. As the quality of sleep is affected, you may experience daytime sleepiness while working or driving.
Symptoms of obstructive sleep apnoea include:
- Excessive daytime sleepiness
- Loud, frequent snoring
- Choking or gasping episodes during sleep
- Episodes where breathing stops during sleep
- Abrupt and frequent awakenings at night
- Feeling unrefreshed after sleep
- Waking up with a headache or a dry mouth
- Frequent urination at night
- Difficulties with concentration at work or studies
- Reduced libido
Obstructive Sleep Apnoea (OSA) - Causes and Risk Factors
What causes obstructive sleep apnoea (OSA)?
Individuals with obstructive sleep apnoea have a narrower upper airway and repeated upper airway obstruction during sleep. This leads to poor sleep quality, sleep deprivation and cardiovascular abnormalities that put tremendous stress on the heart and body.
The upper airway obstruction leads to decreased oxygen supply to the brain, heart and other organs, causing the heart to work harder to provide oxygen to the tissues, leading to medical consequences in the long run.
What are the risk factors for obstructive sleep apnoea (OSA)?
Risk factors for obstructive sleep apnoea include:
- Anatomic abnormality. Snoring and OSA occur because of anatomic abnormality in the upper airway leading to obstruction. The sites involved include the:
- Nose (enlarged turbinates, deviated nasal septum, and nasal polyps)
- Oropharynx (long, redundant and thick palate and uvula, large tonsils)
- Hypopharynx/base of tongue (lingual tonsillar hypertrophy, floppy epiglottis, and bulky tongue) and throat
- Genetics. Genetic predisposition leading to facial and jaw abnormalities are known predisposing risk factors.
- Medications / Alcohol. Mild or intermittent snoring may be a result of medications (like sedatives to help you sleep) or alcohol that induce relaxation of the upper airway muscles.
- Weight. Weight gain can contribute to snoring and OSA. Excessive fat accumulation in the upper airway can amplify an existing anatomic narrowing that was causing mild obstruction previously.
- Gender and Age. The male gender and increased age are risk factors.

Diagnosis of Obstructive Sleep Apnoea (OSA)
How is obstructive sleep apnoea (OSA) diagnosed?
Consult your physician if you have loud snoring or excessive daytime sleepiness despite getting enough sleep. Your physician will evaluate the possible causes and advise on the appropriate management.
You may be referred to a sleep disorders clinic for a comprehensive evaluation of your problem.
Evaluation of obstructive sleep apnoea includes:
- Thorough sleep history
- Physical examination and sleep study.
- Good history consisting of sleep patterns and presence of any snoring or day time sleepiness.
- Examination of the airway via an endoscope to assess for any narrowing of the airway.
- Evaluation usually involves an overnight sleep study.
Given the possible long-term complications of obstructive sleep apnoea, it is important for you to follow-up with appropriate treatment once diagnosed.
The management of obstructive sleep apnoea is multidisciplinary in nature, and may involve specialists from medical specialties such as otolaryngology to dental specialties such as oral and maxillofacial surgery and orthodontics.
What is a sleep study?
A sleep study or inpatient overnight diagnostic polysomnography (PSG) is an overnight non-invasive diagnostic test performed in a sleep laboratory.
Treatment for Obstructive Sleep Apnoea (OSA)
How is obstructive sleep apnoea (OSA) treated?
Continuous Positive Airway Pressure (CPAP)
A medical device called Continuous Positive Airway Pressure (CPAP) is considered the gold standard treatment for Obstructive Sleep Apnoea (OSA). CPAP is safe, generally welltolerated and highly effective.
This device must be worn nightly and long-term CPAP compliance is essential for its effectiveness.
If you are unable to tolerate CPAP therapy, other treatment options include mandibular advancement splints and surgery. These treatment options are described in detail under the following sections.
How Does Continuous Positive Airway Pressure (CPAP) Therapy Work?
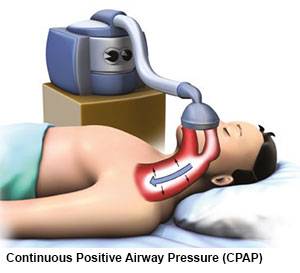
Continuous Positive Airway Pressure (CPAP) therapy works by quietly delivering pressurised air to the nose and back of the throat to prevent the airway from collapsing during sleep.
There are two important parts of the CPAP machine that need to be decided on in careful consultation with your sleep physician, prior to using CPAP.
They are:
1. The Mask
Continuous Positive Airway Pressure (CPAP) is administered through a mask that seals either the nose, the mouth or both.
There are a variety of masks that can be used. Most of these are made from soft silicone or gel to maximise comfort. The mask chosen for you will be fitted by a sleep technician to suit your facial structure and breathing habits. There are different types of masks to suit different needs, such as:
- Nasal masks
- Oral-nasal masks
- Nasal pillows
- Full face masks
- Oral masks
2. The Machine
Most Continuous Positive Airway Pressure (CPAP) machines today are small, quiet and relatively portable. Modern CPAP devices can deliver a fixed pressure, or may have a sophisticated software that can detect obstruction and self-adjust the delivered pressure (autotitrating machines).
The type and setting of each device will need to be individualised for you after consultation with a sleep specialist. An overnight CPAP titration sleep study may be required to determine the settings that are most suitable for you.
Benefits of Continuous Positive Airway Pressure (CPAP)
OSA sufferers who start using CPAP report sleeping better and feeling more energetic and less sleepy during the day.
Some report feeling better after the first day of treatment while for others, the improvement may only become apparent after a few weeks of sustained use.
The benefits of Continuous Positive Airway Pressure (CPAP) include:
- Improved sleep quality
- Improved daytime sleepiness
- Improved memory and cognition
- Improved blood pressure control
- Improvement in bed partner’s sleep with the elimination of your snoring
Common Problems Associated with CPAP
It may take a while to get used to CPAP treatment, but it is important to persevere to reap the benefits of your treatment. Minor troubleshooting may be required, and it may take time to find the right device settings for you.
Some common problems encountered, and troubleshooting tips are as follows:
Dryness of the upper airway
This may occur due to low levels of humidity in the environment or as a result of a mask air leak. The use of a humidifier will help in increasing air moisture, reduce dryness of the airways and increase comfort. It is also important to ensure that your mask fits well to reduce air leak.Mask air leak
Re-adjust the mask if you experience mask air leak during the night. If it persists, work with your doctor and the sleep technologist/ CPAP vendor to find an alternative mask that is more suitable for you.Difficulties in getting used to wearing a CPAP mask
You may wish to try using the CPAP while you are awake for short periods of time in the day, for example, while watching TV. When you are used to how it feels, you may start using the CPAP every time you sleep.Difficulties in falling asleep
If you find the CPAP pressure too high as you are trying to fall asleep, a ‘ramp’ function on the CPAP machine may be used. When this ‘ramp’ function is switched on, the CPAP machine will begin with a low pressure setting, and gradually increase to the targeted level of CPAP pressure as you fall asleep.CPAP pressure is too high
If you feel uncomfortable with the pressures delivered by the CPAP machine during sleep, please highlight this to your doctor. An overnight CPAP titration sleep study may be required to determine the settings that are most suitable for you.
With time, patience and support, CPAP can significantly benefit your overall health and quality of life.
Oral Appliances for Obstructive Sleep Apnoea (OSA)
What is an Oral Appliance (OA) or a Dental Splint?
An oral appliance (OA) or a dental splint is an alternative to the CPAP in managing snoring and mild to moderate Obstructive Sleep Apnoea (OSA). OA looks like the removable functional braces worn by children, or mouth guards that protect the teeth during sports.
There are many names for an OA:
- Mandibular advancement device
- Mandibular advancement splint
- Sleep apnoea mouth guard
- Sleep apnoea dental appliance
- Sleep apnoea oral appliance
An OA is different from a dental splint, that is used to protect the teeth in bruxism (tooth grinding).
Proper examination and diagnosis are needed to determine the jaw structure and nature of airway obstruction, before prescribing an OA. Those who mouth breathe will not be able to use an OA as it fills the oral cavity and obstructs mouth breathing.
Another form of an OA, is the Tongue Stabilising Device (TSD). It also goes by many names: tongue retaining device, sleep apnoea tongue device or tongue guard.
It is a silicone suction cup that clips over the front of the tongue. Lip shields protrude from the device to keep the tongue positioned outside the mouth. The tongue guard holds onto the tongue and prevents it from falling backwards into the airway during sleep.

How Do Oral Appliances (OA) Work?

In oral devices (OAs) such as mandibular devices, there are built-in mechanisms such as screws, connectors or bite blocks, to thrust the mandible (lower jaw) forward. The tongue, soft palate, other muscles and soft tissues in the mouth and throat become stretched and taut as the mandible is re-positioned anteriorly.
With the tongue and soft palate shifted forward and away from the airway, the calibre of the airway increases.
Oral appliances are potentially effective in patients diagnosed with mild to moderate OSA particularly where the airway obstruction occurs at the level of the tongue. Adjustments may be necessary in the first few months.
A customised OA is made of acrylic-like dental splints and is anchored on all teeth in both the jaws.
Sometimes an OA may be used together with a CPAP machine to reduce the air pressure for easier breathing. There is an OA adjustment (titration) period of four to six months, when the mandible is gradually advanced into an optimum position, before a second sleep study is done to determine the effectiveness of the OA.
Side Effects of Oral Appliances (OA)

The common side effects in using an OA are an open mouth posture and drooling during sleep. The jaw muscles and teeth, especially the incisors, may be sore or painful at the start of OA use.
The pain and discomfort will reduce, after a wearing-in period of up to six months. The way the teeth fit together may change, and the lower teeth will bite in a more forward position in the morning. The change in bite is transient and lasts for an hour or so after the removal of the OA.
However, after many years of long-term use, there may be a small permanent change to the lower jaw position which becomes a couple more millimetres forward; it does not make a big visible change to the physical appearance.
The horizontal gap between the upper and lower incisors may be reduced, and the lower incisors will shift to an edgeto- edge bite with the upper incisors. The bite of the molars will also change after a couple of years.
If oral hygiene practice is poor during OA use, tooth cavities and tooth loosening may occur. Dental fillings, crowns, bridges, implants and gum treatment should be done first before the OA is made.
An OA does not last forever. It may be necessary to replace an OA every three to five years depending on the maintenance of the OA and whether it still fits.
Advice to Oral Appliance (OA) Wearers

An OA cannot be worn if there is poor oral health maintenance. Teeth are anchors for the OA, and OSA management is not effective when teeth are loose or lost through a lack of oral healthcare.
Sleep studies are necessary every few years to determine if the OA is still effective. OA treatment becomes less effective with weight gain and increased severity of OSA.
The following are advised in OSA treatment using an OA:
- Maintain good oral health and have a dental check-up every six months.
- Make sure the nasal passage is patent for breathing through the nose.
- Exercise regularly and keep to a healthy weight in the BMI range below 23.

Mandibular Advancement Splints
Mandibular Advancement Splints: What To Expect
In the first few weeks. You will find the mandibular advancement splint very uncomfortable. Your lower jaw is held forward during the night and you will experience aching of the jaw muscle in the first few hours of the morning. You will also feel as though your teeth do not fit together properly. These symptoms usually disappear by noon.
During sleep. You will experience a lot of saliva and drooling in the first few weeks of wearing the splint. You may want to sleep with a handkerchief or towel on your pillowcase. Sometimes, you will wake up to find that you have unknowingly removed the splint during sleep.
These initial problems will gradually go away after a while. To make it easier for you to get used to the splint, put it on 1 to 2 hours before you go to sleep.
In most cases, snoring will be reduced to an acceptable level or it will disappear. The number of apnoeas or cessations of breaths per hour will be reduced to a less harmful level.
The application may take several weeks to become effective. This is because the tissues of the airway may have been damaged from prolonged snoring. If you have daytime sleepiness, it will take a few weeks before you notice the difference and begin to feel good.
After you have used the splint for some time, you can sleep without it for one to two nights a week and the positive effects continue to stay with you.
Mandibular Advancement Splints: Adverse Effects
If you have had joint problems with clicking and pain before, these problems can return and your splint will have to be altered. This is because your jaw-joints and your teeth support the forward position of your lower jaw.
If you have a new filling or crown made, alterations of the splint is necessary.
If you have gum disease, support for your teeth is not as strong and your teeth can shift. It is important to make regular visits to your dentist in order to keep your gums healthy and to prevent cavities from developing in your teeth.
Long term wear of the splint may alter the way your teeth meet. The over jet and overbite of your front teeth will be reduced. There will be a mild increase of the lower face height.
The side effects are minor and outweigh the effects of the splint.
Surgery for Obstructive Sleep Apnoea (OSA)
Do I need surgery for obstructive sleep apnoea ?
Surgery is indicated for OSA when first-line treatment, such as behavioural and lifestyle modifications, CPAP therapy as well as dental appliances, have failed. Surgery is also recommended, when you have easily correctible abnormalities of the upper airway, such as enlarged tonsils and adenoids.
Patients may also need nasal surgery if they have nasal congestion affecting CPAP usage.
Planning for OSA Surgery
Pre-surgical assessment should include:
- Polysomnography
- A detailed history with head and neck physical examination
- Fiber-optic endonasopharyngoscopy
- Appropriate imaging study and sleep endoscopy
They will enable the surgeon to have enough information to help in individualising surgical treatment depending on the severity and sites of obstruction. The surgeon will not rely on a single test or procedure to decide on the treatment.
Successful surgical therapy for treating OSA is based on identifying the levels of airway obstruction, usually in multiple sites, which may include regions of the nose, soft palate and tongue base. No single surgical procedure can guarantee success.
Surgical procedures serve to remove or reposition tissues that partially or completely block the upper airway during sleep. These procedures have been used for years and clinical outcomes have verified their use.
All cases for surgery are examined thoroughly in order to customise the treatment plan. In many instances, the multidisciplinary approach is taken and a team of surgeons is brought in for combined surgery. Sometimes, it may be necessary to stage surgical treatment into separate surgeries done at different times.
Other investigations to evaluate the upper airway may be performed, including:
- Lateral cephalometry
- Computed tomography (CT) or magnetic resonance imaging (MRI) scans of the upper airway, awake or asleep
- Drug-induced sleep endoscopy
- Computer-assisted airway measurements (CAM)
Types of Surgery for Obstructive Sleep Apnoea (OSA)
The purpose of surgery is to reduce, remove or reposition tissues of the upper airway, in order to increase the upper airway dimensions and reduce obstructions.

There are numerous surgical options for the treatment of OSA for patients who have failed CPAP therapy. Everyone has a different upper airway and a different cause of OSA. A single surgical treatment protocol will not work for all.
Surgery needs to be individualised to each and every single patient to ensure that unnecessary surgery is not performed. The most conservative surgical option is also the most effective.
1. Nasal Surgery
In the nose, normal structures like the turbinate may be enlarged due to allergic rhinitis. The nasal septum that divides the nose into the left and right sides may also be deviated to one side.
Sinusitis, nasal polyps and enlarged adenoids can also contribute to nasal obstruction which results in mouth breathing.
This causes the tongue to fall backwards, contributing to upper airway obstruction. Nasal obstruction also reduces CPAP compliance due to nasal discomfort.
Treatment of nasal obstruction begins with allergen avoidance, medications like antihistamines, intranasal steroids, nasal decongestants and antibiotics when required. Nasal surgery is indicated when medical therapy fails.
Surgical options to relieve nasal airway obstruction include:
- Reducing the size of the turbinates
- Straightening the deviated nasal septum
- Removing enlarged adenoids
- Endoscopic sinus surgery to treat nasal polyps and sinusitis

2. Palatal Surgery

The area behind the soft palate is the most common site of obstruction, contributing to snoring and OSA.
This is usually a result of bulky, floppy, low-lying soft palate, enlarged tonsils, excessive posterior tonsillar pillar muscles or mucosa, elongated uvula and redundant lateral pharyngeal mucosa.
For those with snoring and mild or moderate OSA, radiofrequency ablation of the soft palate may be performed under local anaesthesia, to reduce the floppiness and bulkiness of the soft palate.
Alternatively, tonsillectomy and uvulopalatopharyngoplasty (UPPP) or one of its many variations can be performed under general anaesthesia to increase the airway dimensions behind the soft palate.
Some of the variations of UPPP include:
- Uvulopalatal flap
- Relocation pharyngoplasty
- Lateral pharyngoplasty
- Barbed reposition pharyngoplasty
3. Hypopharyngeal and Base of Tongue Surgery
The base of the tongue and lingual tonsils (lymphoid tissue at the base of tongue) may be enlarged, contributing to upper airway obstruction during sleep.
The epiglottis (cartilage situated behind and below the base of the tongue) can also cause airway obstruction during sleep. Some people may have a small lower jaw that leaves less room for the tongue, resulting in posterior displacement of the tongue, reducing the size of the upper airway.
Options to treat obstruction, include both soft tissue surgery as well as bony skeletal surgery. Soft tissue surgery involves radio frequency ablation to reduce the size of the tongue, or median glossectomy to remove the middle portion of the back of the tongue.
Transoral Robotic Surgery (TORS) can be used to access the back of the tongue, allowing for superior access and view of the tongue base and hypopharyngeal area.

Bony skeletal surgery to the lower jaw can also be performed to increase the airway size behind the tongue, and increase tension on the tongue to prevent it from falling backwards and causing obstruction during sleep. Examples of such surgeries include:
- Sliding genioplasty
Surgery to cut and reposition a part of the chin bone towards the front. - Genioglossus advancement
Surgery where the tongue is pulled forward. - Hyoid suspension
Surgery where the hyoid bone (U-shaped bone in the front midline of the neck) and its muscle attachments to the tongue and airway are pulled forward.
4. Maxillomandibular Advancement Surgery
Maxillomandibular advancement (MMA) is a more invasive but effective surgery, with up to a 90 percent success rate.
This procedure is performed in severe OSA cases when nasal, palate and tongue base surgeries are not effective enough. It is a major surgical procedure where both the upper and lower jaws are surgically advanced using orthognathic surgery techniques, increasing the space behind both the palate as well as the tongue base. It is done in conjunction with fixed orthodontic braces to shift the upper and lower teeth into a good bite after the surgery.
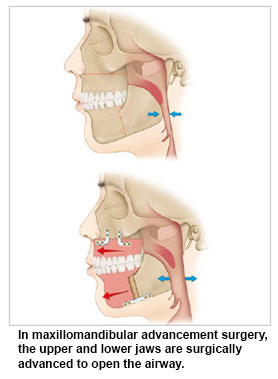
The duration of treatment may take as long as one to three years. All soft tissues and muscles attached to the jaws are brought forward. This pulls on the lax soft tissues to tighten them up.
The airway and larynx open up and become much bigger when the soft palate and tongue are relocated anteriorly after surgery. Long-term studies show a high success rate in managing OSA with this procedure, which also achieves good quality of life outcomes.
5. Hypoglossal Nerve Stimulation

Hypoglossal nerve stimulation is a novel form of therapy in treating OSA by increasing upper airway muscle tone during sleep.
This is achieved by implanting a device beneath the skin in the chest. This device is switched on by the patient just before sleep, and it applies mild stimulation to the hypoglossal nerve that supplies the tongue. This achieves optimal tongue protrusion required to prevent tongue base obstruction during sleep.
6. Tracheostomy
Tracheostomy involves creating a hole in the windpipe (trachea) in the lower part of the neck to bypass the upper airway obstruction. The patient, thereafter, will be breathing through the hole in the lower neck during sleep.
A tracheostomy tube may be placed through this hole to help with the breathing. It is used in people with refractory airway obstruction, and in the morbidly obese with medical conditions that contraindicate surgeries that are more extensive.
Although this is a simple procedure with a success rate of almost 100 percent, this option is poorly accepted by patients, due to the stigma and problems that comes with breathing through a hole in the lower part of the neck.
Treating Obstructive Sleep Apnoea (OSA) at Home
Lifestyle changes can help in mild cases of obstructive sleep apnoea (OSA). You can:
- Sleep on your side to reduce the incidence of apnoea during sleep
- Lose weight if you are obese
- Exercise regularly
- Quit smoking
- Avoid consuming alcohol at night. Alcohol causes relaxation of the upper airway muscles.
- Avoid sleeping pills/sedatives as these may cause relaxation of the upper airway muscles.
Myofunctional Therapy and Nasal Breathing Exercises
Obstructive Sleep Apnoea (OSA) - Other Information
Is obstructive sleep apnoea dangerous and must it be treated?
Obstructive sleep apnoea has been linked to increased chances of heart disease, stroke, and irregular heart rhythms. Unfortunately, not all the long term effects of untreated sleep apnoea are known today. However, continual lack of refreshing sleep can lead to depression, irritability, lack of energy, a high risk of motor vehicular accidents, workplace accidents and many other problems. Most specialists agree that obstructive sleep apnoea is dangerous and should not be ignored.
If I have sleep apnoea, how can I help myself?
Besides seeking medical attention, there are several things doctors suggest you can do to alleviate obstructive sleep apnoea including weight loss, quitting smoking, eliminating alcohol and avoiding sedatives especially before bedtime.
I don't awake repeatedly throughout the night. Does it mean I do not have sleep apnoea?
No. Most people with sleep apnoea do not realise that they are awakening to breathe repeatedly throughout the night. This is because the arousal is slight and most people become accustomed to this. However even this slight arousal is enough to disrupt the pattern of sleep and lead to unrefreshing sleep.
What should I do if I think I may have sleep apnoea?
The best thing is see your doctor. He may refer you to a specialist or sleep disorders unit for you to undergo evaluation which may include spending the night in a sleep lab to undergo a sleep study call polysomnogram.
References
- Obstructive sleep apnoea (OSA). Asthma + Lung UK. (n.d.). https://www.asthmaandlung.org.uk/conditions/obstructive-sleep-apnoea-osa
- Foundation, S. H. (2024, January 12). Obstructive sleep apnoea (OSA). Sleep Health Foundation. https://www.sleephealthfoundation.org.au/sleep-disorders/obstructive-sleep-apnoea
- Verbraecken, J. (2023). Epidemiology of obstructive sleep apnoea, central sleep apnoea and hypoventilation syndromes. ERS Handbook of Respiratory Sleep Medicine, 38–43. https://doi.org/10.1183/9781849841641.008022
- Steier, J. (2022). Novel approaches for the treatment of obstructive sleep apnoea. Oxford Handbook of Sleep Medicine, 111–118. https://doi.org/10.1093/med/9780192848253.003.0012
- Robinson, T., & Scullion, J. (2021). Obstructive sleep apnoea. Oxford Handbook of Respiratory Nursing, 335–344. https://doi.org/10.1093/med/9780198831815.003.0013
Contributed by
The information provided is not intended as medical advice. Terms of use. Information provided by SingHealth.
Condition Treated At
Department
Department of Oral & Maxillofacial Surgery
Department
Department of Orthodontics
Department
Otolaryngology (ENT)
Department
Otorhinolaryngology - Head &Neck Surgery
Department
Sleep Disorders
Department
Otorhinolaryngology- Head & Neck Surgery
Department
Sleep Medicine, Surgery & Science
Department
Otolaryngology (ENT)
Department
Department of Respiratory Medicine
Department
Sleep Clinic
Department
Department of Surgery
Department
Internal Medicine
Get to know our doctors at SingHealth Hospitals in Singapore.
Get to know our doctors at SingHealth Hospitals in Singapore. here.





















