What is
What is breast cancer?

Breast cancer is the most common type of cancer among women in Singapore today. 1 in 12 women in Singapore is likely to develop breast cancer in their lifetime*.
*Source: National Registry of Diseases Office. (2024). Singapore Cancer Registry Annual Report 2023.
Normal cells divide and reproduce in an orderly manner. Your body relies on this orderly activity to repair injuries and replace wornout tissue. Sometimes this orderly process is disrupted. Cells grow and divide out of control, producing extra tissue to form a mass or lump called a tumour. A tumour can be benign or malignant.
Benign tumours are not cancers. They may grow slowly but do not spread to other parts of the body.
Malignant tumours are cancerous growths and have the potential to spread to other parts of the body.
Breast cancer is a malignant tumour which occurs when breast cells become abnormal and divide without control or order.
The majority of breast cancers start in the milk ducts. A small number start in the milk sacs or lobules. Within these two groups, some grow very slowly while others develop more rapidly.
Breast cancer can spread to the lymph nodes and to other parts of the body such as the bones, liver, lung and sometimes to the brain.
Screening
How can breast cancer be detected early?
Screening simply means performing a procedure or test to detect an abnormality before symptoms appear. This allows problems to be detected earlier, investigated and treated early.
Breast screening methods include:
A. Breast Self-Examination Breast Self-Examination (BSE)
BSE is recommended once a month about 1 week from the first day of menses. For women who no longer menstruate, choosing a date each month is an easy way to remember. Report to the doctor any breast changes such as redness, swelling, presence of a lump, skin changes or discharge from the nipple.
Self-awareness of breast changes through regular BSE and being familiar with what is normal and stable is useful to detect abnormalities.
HOW TO PERFORM BREAST SELF-EXAMINATION
- Look for changes in front of a mirror
- First, with arms at your sides
- Next, with arms raised above your head
- Finally, with hands pressed firmly on hips and chest muscles contracted

- First, with arms at your sides
- In each position, turn slowly from side to side and look for:
- Change in size or shape of your breasts
- Dimpling of the skin
- Change in nipples
- Feel for the changes lying down
- Put a small pillow under yourright shoulder
- Place your right hand under your head
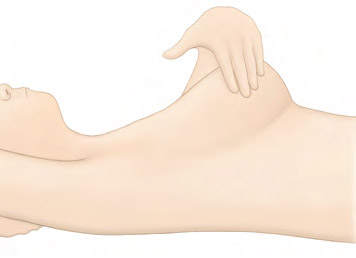
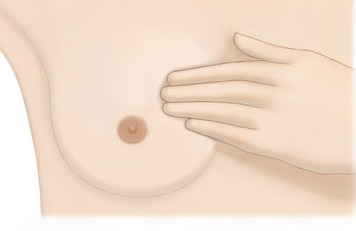
- Use the pulp of your left fingers to feel for any lumps or thickeningin your right breast
- Feel for the changes lying down
- First, feel the armpit
- Then start on the outside edge of your breast and feel round the whole breast in smaller and smaller circles
- Finally, feel behind the nipples itself
- Look for bleeding or discharge from the nipple
- Squeeze the nipple gently to see if there is bleeding or any discharge

- Squeeze the nipple gently to see if there is bleeding or any discharge
- Repeat step 2 and step 3 for the left breast.
B. Clinical Breast Examination
Have a doctor or breast specialist nurse examine your breasts once every year if you are 40 years and above. This includes a visual examination and a manual check of the entire breast and underarm area for changes. Changes in the breast may not be due to cancer and diagnostic tests may be performed to assess these changes.
C. Mammogram Screening
Mammography is a low-powered X-ray technique that gives an image of the internal structure of the breast. Usual screening mammograms involve taking X-ray images with the breast compressed between two plates with two views taken — cranial caudal or horizontal and mediolateral oblique or diagonal.

Mammograms take an image of the internal structure of the breast and can help detect abnormalities.
Additional angles and magnified views may be taken if there are areas of concern. It can detect the presence and position of abnormalities and help in the diagnosis of breast problems, including cancer.
The risk of developing breast cancer increases with age. Women with risk factors such as a family history of breast cancer should discuss with their doctors when to go for and the interval of regular screening.
There are other tests such as breast ultrasound, tomosynthesis and MRI, available for assessment of the breasts.
These are not used for regular screening in well women and are used for further evaluation after initial screening mammogram, but may be considered for women with high risk of breast cancer.

Symptoms
What are the symptoms of breast cancer?
Ductal carcinoma in situ (DCIS) generally does not cause symptoms, and is most commonly discovered in screening mammograms. Occasionally, women with Ductal carcinoma in situ (DCIS) may present with a breast lump or bloody nipple discharge.
Breast cancer is otherwise usually painless and there may be no symptoms in the early phase when breast cancer first develops.
When the cancer grows, signs and symptoms may develop and they can include:
- A persistent lump or thickening in the breast or in the axilla
- A change in the size or shape of the breast
- A change in the colour or appearance of the skin of the breast such as redness, puckering or dimpling
- Bloody discharge from the nipple
- A change in the nipple or areola, such as a persistent rash or nipple retraction (nipple pulled into the breast)
Prevention
What are some ways to reduce the risks of breast cancer?
There is no sure way to prevent breast cancer, but the risks can be lowered. These include modifying the risk factors which we have control over such as:
- Exercise and increasing physical activity
- Limiting alcohol intake
- Keeping a healthy diet to prevent obesity, especially post-menopause
- Cease smoking. Smoking increases the risk of many other cancers and is bad for overall health. There are suggestions of links between smoking and breast cancer
- Have more children if one is able to
- Limit the use of HRT and OCP
- Limit your exposure to environmental pollution and radiation such as the use of medical imaging like computerised tomography (CT) scans unless really necessary
In high-risk women, such as those with a very strong family history or have genetic mutations such as the BRCA, risk-reducing options include taking drugs or having surgery that can reduce their risk. Risk-reducing surgeries include removal of the breast (mastectomy) and removal of the ovaries.
An alternative management strategy to risk-reduction methods is close surveillance. While this does not reduce the risk of cancer development, it does improve outcome by discovering the cancers in earlier stages, allowing earlier treatment and hence better outcomes.
Genetic Risk Assessment for Hereditary Breast Cancer & Implications
What is Hereditary Breast and Ovarian Cancer (HBOC) syndrome?
About 5 to 10 percent of breast cancers can be attributed to hereditary breast and ovarian cancer (HBOC) syndrome. Genetic change (mutation) in the BRCA1 or BRCA2 gene is the most common cause of Hereditary Breast and Ovarian Cancer (HBOC).
Individuals with BRCA1 or BRCA2mutation tend to develop cancer at an earlier age than the general population and have higher risk for bilateral breast cancer, a second primary tumour in a different tissue, and cancer recurrence.
Mutations in other less common genes have also been found to increase the risk of developing breast and other cancers.
Who might be at risk?
Hereditary Breast and Ovarian Cancer (HBOC) is an adult-onset, cancer predisposition syndrome which can be passed down through generations.
The history of cancer in your close relatives is a clue about the chance of HBOC syndrome in your family. It is more likely if one or more of the following features can be confirmed in your family:
- Young age of onset
- Bilateral breast cancer or personal history of multiple cancers
- Family history of ovarian, peritoneal, fallopian tube, pancreatic cancers and/or melanoma
- History of male breast cancer in the family
How is Hereditary Breast and Ovarian Cancer (HBOC) syndrome diagnosed?
Genetic testing for Hereditary Breast and Ovarian Cancer (HBOC) syndrome is a blood test that is available at the Cancer Genetics Service at NCCS when specific criteria are met. Genetic testing is complex, thus it does not take place without genetic counselling and the process of informed consent.
What does genetic counselling involve?
Cancer genetic counselling is a process to assess a person's risk of having an inherited susceptibility to cancer. It is usually provided by a genetic counsellor and/or cancer geneticist to help people understand and adapt to the medical, psychological and familial implications of genetic contributions to cancer.
Genetic counselling can help you better understand the outcomes and impacts of genetic testing and the possible implications when finding a genetic mutation of Hereditary Breast and Ovarian Cancer (HBOC) syndrome.
What can I do to reduce my risk of developing breast or ovarian cancer if I have a BRCA gene mutation?
Increased surveillance (clinical breast exam, mammogram and MRI) and consideration of risk-reducing interventions (such as chemoprevention and preventive mastectomy or oophorectomy) are recommended.
What should I do if I am concerned?
If your family history of cancer suggests Hereditary Breast and Ovarian Cancer (HBOC) syndrome, please talk to your doctor regarding your concerns and they will make the necessary arrangements if a genetic risk assessment is needed.
What are the implications of genetic testing for HBOC?
Finding a genetic mutation of Hereditary Breast and Ovarian Cancer (HBOC) syndrome may help to:
- Inform family members about their own cancer risk
- Direct appropriate cancer screening and risk-reduction options for affected patients and family, and avoid unnecessary testing in those who do not require increased surveillance
- Explain the history of cancer in a family
Causes & Risk Factors
What causes breast cancer?
The causes of breast cancer are not exactly known but there are risk factors that increase the chance of developing breast cancer.
What are the risk factors of breast cancer?
Having risk factors do not mean a woman will definitely develop breast cancer, as many women who have had breast cancer did not have any apparent risk factors.
Some risk factors such as gender and age, or those related to our environment cannot be changed (non-modifiable), while others are modifiable as they are related to our lifestyle choices.
Non-modifiable Risk Factors
- Age and gender
- Early menarche, late menopause
- Family history and genetic factors
- Previous breast cancer
- Certain breast changes in biopsies (such as atypical ductal hyperplasia and LCIS)
- Radiation exposure for medical reasons
Being a woman is a risk factor for developing breast cancer. Women have a much higher chance of developing breast cancer than men due to the female hormones oestrogen and progesterone.
This risk is increased with longer hormonal exposure in women with early menarche (onset of menstruation) before the age of 12 and late menopause (after the age of 55).
Other hormonal-related factors include never having children, late childbearing (after the age of 30), and obesity, especially excessive weight gain in post-menopausal women. This risk also increases with age.
Genetic factors and family history of breast cancer, especially in a first-degree relative (mother, sister or daughter), or two or more close relatives such as cousins and the presence of genetic alterations in certain genes such as BRCA1 and BRCA2 which are associated with significant lifetime risks of breast cancer.
A past history of breast cancer, radiation exposure for medical reasons and certain benign conditions such as atypical ductal hyperplasia, atypical lobular hyperplasia or lobular carcinoma in-situ diagnosed on breast biopsy also increase the risk.
Modifiable Risk Factors
- Lack of exercise
- Excessive alcohol consumption over a long period of time
- Smoking
- Use of oral contraceptive pills (OCP) and combined hormonal replacement therapy (HRT) over a long period of time
However, most women who have breast cancer have none of the above risk factors. Likewise, not possessing any of these risk factors does not mean that one will not get breast cancer. There is ongoing research to learn more about these factors, as well as ways to prevent breast cancer.
Diagnosis
What are the types of breast cancer?
Breast cancer can be classified by:
- the stage of cancer at diagnosis and
- their biological characteristics.
These will determine treatment recommendations as it has prognostic (most likely outcome of the disease) implications and treatment implications.
I. Staging
Understanding the stage of the cancer is important to understand the prognosis and the treatment recommendation.
Cancers treated in earlier stages have better outcomes, more advanced cancers will need more aggressive treatment.
Cancer stage is based on:
- Whether the cancer is non-invasive or invasive
- The size of the invasive cancer
- Whether the cancer has spread to the lymph nodes
- Whether the cancer has spread to other parts of the body
The TNM staging system is based on:
T: Size of the tumour
N: Lymph node involvement
M: Metastasis when cancer has spread to other organs like the lung, liver and bones. Different T, N and M in combination will determine the stage of the cancer.
Stage 0 or Ductal Carcinoma in Situ (DCIS) is a common non-invasive breast cancer, where cancer cells are still within the ducts and have not grown out to breach the duct linings into the surrounding normal breast tissue.
DCIS, also known as Stage 0 breast cancer, unlike invasive breast cancer, is not life-threatening, but it can increase the risk of developing an invasive breast cancer.
lnvasive breast cancer occurs when cancer cells spread beyond the ducts or lobules resulting in invasive ductal and invasive lobular breast cancer, the two most common subtypes of breast cancer.
Metastatic breast cancer refers to the stage when the cancer has spread beyond the breast to distant organs such as the lungs, liver or bones.
II. Tumour Biology
Breast cancers are also differentiated by the presence of special receptors on the surface of the cancer cells, such as the:
- Oestrogen receptor
- Progesterone receptor
- HER2 (Human Epidermal Growth Factor 2) receptor
This is associated with the aggressiveness of the cancer and affects the prognosis of the patient.
More importantly, there are drugs to target these changes, and hence directed treatment for them will improve the outcome.
The histopathological (microscopic appearance) subtype of the cancer also helps to determine the prognosis, and nature of breast cancer overall.
The grade (assessment of how abnormal the cancer cells look) also determines the aggressiveness and hence, treatment recommendations.
The most common subtype is the invasive carcinoma of no special type (NST). Specific subtypes include invasive lobular, tubular, cribriform, metaplastic, apocrine, mucinous, papillary andpillaryarcinoma, as well as carcinoma with medullary and neuro micropaendocrine (WHO classification 2012).
How is breast cancer diagnosed?
If there is an unusual lump or changes in the breasts, seek medical attention. Try to pinpoint the area accurately as this will assist the doctor with the examination. Tests will be recommended to obtain a definite diagnosis.
Tests to diagnose Breast Cancer include:
1. Imaging
a. Mammogram
Mammography is a low-powered X-ray technique that gives a picture of the internal structure of the breast. Usual screening mammograms involve taking X-ray images of the breast compressed between two plates with two views taken — cranial caudal or horizontal and mediolateral oblique or diagonal.
Additional angles and magnified views may be taken if there are areas of concern. It can detect the presence and position of the abnormalities and help in the diagnosis of breast problems, including cancer.
Any previous mammograms (and reports if available) should be brought along when seeing a doctor.
Sometimes a lump that can be felt is not seen on a mammogram. Other tests may be necessary to determine if the lump is cancerous.

b. Ultrasound
Breast ultrasound is the use of high-frequency sound waves to produce an image of breast tissue.
The sound waves are transmitted from the probe through the gel into the body. The transducer collects the sounds that bounce back and a computer then uses those sound waves to create an image.

c. Magnetic Resonance lmaging (MRI)
This uses a combination of magnetism and radio waves to build up a picture consisting of detailed cross-sections of pictures of the breasts.
The test involves lying on the stomach on a padded platform, with cushioned openings for the breasts, that passes through a tunnel-like structure (which forms a very large magnet). It may take up to one hour to complete, but is completely painless.
Magnetic Resonance lmaging (MRI) is useful when mammograms are not suitable, e.g. in young women with dense breast tissue or when findings on mammograms and ultrasound are not conclusive to achieve a diagnosis.
It is used as a screening tool for young women with high-risk factors like BRCA gene carriers or those with a very strong family history of breast cancer.

d. Tomosynthesis
This involves taking multiple X-rays of each breast from many angles. The breast is positioned the same way as in a conventional mammogram, but only a little pressure is applied, just enough to keep the breast in a stable position during the procedure.
An X-ray tube moves in an arc around the breast while images are taken. Information is sent to a computer, where it is assembled to produce clear, highly-focussed 3-dimensional images throughout the breast.

2. Biopsy
a. Core Needle Biopsy
This is a minimally invasive method that obtains a few tiny strips of tissue from an area of abnormality with a wide bore needle. Local anaesthetic is injected to numb the breast area, followed by a small incision in the skin to allow easy insertion of the needle.
If the abnormality is non-palpable (not detectable by clinical examination) and visible on the ultrasound, ultrasound guidance is used to obtain the tissue. Usually 2 to 6 cores of tissue will be obtained for examination.
A nurse will apply compression to the breast to stop any bleeding. The wound is closed by a steristrip and the dressing applied. Strenuous activity is to be avoided for 2 days after the biopsy.

b. Vacuum-assisted Core Needle Breast Biopsy
Vacuum-assisted biopsy (VAB) devices use a larger bore needle with a vacuum component to obtain tissue samples from non-palpable lesions.
Like the usual core biopsy, this minimally invasive procedure is also performed under local anaesthesia, which is injected to numb the breast area, followed by a small incision in the skin to allow easy insertion of the needle. It is used for lesions seen by mammography (stereotactic-guided biopsy), ultrasound or MRI.
The surgeon or radiologist places the probe into the suspicious area of the breast accurately. A vacuum then draws the tissue into the probe, a cutting device removes the tissue sample and then carries it through the probe into a collection area.
More tissue is usually obtained using the Vacuum-assisted biopsy (VAB) than the usual core needle biopsy and the number of strips removed is dependent on the area that needs to be examined.
A small titanium clip (microclip) may be placed at the biopsy site as a location marker for future treatment. This clip is very small (2 mm), is harmless, and will not cause any problems when left inside the breast. An X-ray is taken post-biopsy to ensure proper clip placement. New biodegradable markers are also available now.
A nurse will apply compression to the breast to stop any bleeding, the wound is closed by a steristrip and the dressing applied. Strenuous activity is to be avoided for 2 days after the biopsy.
This procedure is minimally invasive as compared to an open surgical biopsy. It is performed as a day surgery procedure. lt has the ability to sample tiny abnormalities called microcalcifications, making early diagnosis of breast cancer possible.
Under local anaesthesia, it takes about 30 to 45 minutes to complete. The procedure is usually not painful but you may experience some discomfort.

c. Fine Needle Aspiration (FNA)

A syringe with a very fine needle is used to withdraw fluid or cells from a breast lump. This is a simple procedure and can be uncomfortable but is usually tolerable enough for it to be done in the clinic.
If the lump is just a cyst, withdrawing fluid in this manner will usually make the cyst disappear.
However, if the lump is solid, your doctor may use this procedure to withdraw some cells from it. The cells will then be sent to a laboratory for examination.
d. Excision Biopsy
An excision biopsy is the removal of a lump or sample of suspicious tissue by surgery for examination under a microscope to give a definite diagnosis.
For lesions that are small or not palpable, accurate marking of the area for surgery is necessary. These include using ultrasound during surgery, or with procedures done just before surgery to mark the area to be operated.
Ultrasound, mammogram or MRI can be used to insert a small thin wire to the abnormal spot in the breast.
This wire is used to guide the surgeon to remove the area accurately. This technique is known as Hook Wire Localisation (HWL) Biopsy.

Excision biopsies are often performed under general anaesthesia, depending on the size and position of the lump, but local anaesthesia may be used for small lesions close to the skin.
As a minor day surgery procedure, patients can return home after surgery. Strenuous activity is to be avoided for the first few days; immediate ability for usual light activities of daily living is expected.
Post-operative advice may differ between individuals depending on their needs and circumstances. In general, most will be able to return to work in a week.
Treatment
How is breast cancer treated?
Treatment of breast cancer often involves more than one therapy, and may be a combination of therapies.
Treatment recommendations depend on factors such as the cancer type, stage of the cancer, size of the tumour in relation to the breast size, whether breast preservation is desired and the patient’s general health.
Personal preferences determine certain choices, if the option is available, such as the options for the type of surgery. Being diagnosed with breast cancer and having to decide on the treatment options may be difficult. The support of friends and family during the consult and discussion on the results of tests and treatment is recommended.

Local and Systemic Therapy
- Local therapy includes surgery and radiotherapy. It treats the cancer at the site e.g. the breast and axilla (armpit) without affecting the rest of the body.
- Systemic therapy refers to the use of drugs which enter the bloodstream to reach the rest of the body, targeting cancer cells anywhere in the body. Chemotherapy, hormone therapy, and targeted therapy are systemic therapies.
In early breast cancer, surgery is the first treatment of choice. Chemotherapy, targeted and hormonal therapy may be used before surgery (neoadjuvant therapy), or after surgery (adjuvant therapy). Radiotherapy is usually given after surgery.
In stage IV cancer, the goal is to stabilise the disease with systemic therapy. However, local treatment of tumours with radiation therapy or surgery may be recommended when symptoms need to be alleviated.
LOCAL THERAPY FOR BREAST CANCER
Surgery
Surgery for breast cancer is considered in two parts: breast and axillary lymph nodes.
I. Surgery (Breast)
The two broad options are breast-conserving surgery (BCS) or mastectomy.
1. Breast-Conserving Surgery (BCS)
- Wide Excision Breast-Conserving Surgery
In this surgery, the breast cancer and a rim of normal surrounding breast tissue are removed. The breast will remain; a scar and some changes in shape and size of the breast are expected. Patients can go home on the same day or the next day.
After recovering from breast-conserving surgery, radiation therapy to the breast (Mon to Fri) for 3 to 6 weeks is recommended. It helps to reduce the risk of recurrence.
A second operation is needed if cancer cells are noted at the edge in the histological (microscopic) assessment of the removed portion. This occurs in 10 to 15 percent of patients.

- Oncoplastic Breast-Conserving Surgery
In some patients undergoing breast-conserving surgery, additional procedures may be recommended to prevent severe deformities of the breast.
- Breast-Conserving Surgery with Mammoplasty (Reshaping with Breast Uplift / Breast Reduction)
To avoid significant breast deformity after breast-conserving surgery (wide excision), breast reshaping (mammoplasty) may be performed. This is possible if the patient has sufficient remaining breast volume, and often takes the form of a breast uplift or breast reduction. Excess skin may need to be removed, and the exact scar depends on the size of cancer removed and the patient’s existing breast shape.
The most common scars are illustrated (below). If a large reduction is needed, and significant asymmetry in breast volume is anticipated, surgery to the opposite breast may be performed to improve final breast symmetry. This may be performed at the same surgery or as a delayed procedure after cancer treatment.

- Partial Breast Reconstruction – Volume replacement with a local perforator flap
Fatty tissue next to (or below) the breast is used to fill the space in the breast as a result of cancer removal. This maintains breast volume and contour, maintains the nipple position and greatly reduces breast deformity.


- Breast-Conserving Surgery with Mammoplasty (Reshaping with Breast Uplift / Breast Reduction)
Image-Guided Localisation for Surgery
For non-palpable tumours that need to be removed with surgery, localisation with a hookwire or a localising substance under image guidance done prior to the surgery is needed.
This procedure is performed under local anaesthesia, prior to surgery. Mammogram, ultrasound or MRI guidance is used to accurately locate the site for surgery.
A fine wire (hookwire) is inserted or a radioactive substance is injected into the breast, within or in close proximity to the lesion of interest, which will be removed during the surgery.

2. Mastectomy
Mastectomy is the removal of the whole breast (incorporating the breast tumour). In general, there are two types of mastectomy:
- Simple Mastectomy
In a simple mastectomy, the breast, including the nipple-areola complex is removed. After surgery, the chest is flat, with a scar across it. A drain, which is a soft tube, is placed during surgery with the accompanying bottle to remove blood and tissue fluid accumulated at the operated site.
The drain will be removed when the drainage is less than 30 ml a day after 1 to 2 weeks. Drain and wound care will be taught to patients and their caregivers before discharge and patients can go home the next day.

- Mastectomy with Whole Breast Reconstruction
Breast reconstruction is surgery to ‘recreate’ a breast using one's own body tissue or implant after mastectomy. It provides the breast shape, but has no natural feeling.
- Immediate breast reconstruction is when reconstruction is done at the time of mastectomy.
- Skin-sparing mastectomy is where most of the skin of the breast will be preserved.
- Nipple-sparing mastectomy is considered for suitable cases, where the nipple may be preserved if tissue from the base of the nipple shows no cancer cells when tested at the time of surgery. However, if the final histology results show cancer cells behind the nipple, a simple surgery to remove the nipple will be recommended.
- Delayed breast reconstruction may also be done at a later stage, separate from the initial breast surgery.
- Immediate breast reconstruction is when reconstruction is done at the time of mastectomy.
Types of Post-Mastectomy Reconstructions
i. Flap reconstructions
Skin, fat and sometimes muscle (a flap) from another part of your body may be used to make into a breast shape. This operation takes about 6 to 8 hours and requires a hospital stay of between 1 to 2 weeks. Several drains are used and removed after 1 to 2 weeks. Flaps may be from the following areas:
- Back (latissimus dorsi)
- Buttock
- Thigh
- Abdomen
- TRAM (transverse rectus abdominis myocutaneous) flap
- DIEP (deep inferior epigastric perforator) flap, taking skin and fat only

Additional procedures to improve the look of the breast after the initial surgery may include adding a nipple, surgery to the opposite breast to create a good match, or refining the shape of the recreated breast.
ii. Breast implants
Silicone implants may be used to create a new breast and the operation takes about 4 to 5 hours. There are usually 2 to 3 drains inserted and the hospital stay is 2 to 5 days.
A 1-stage procedure is when the permanent implant is inserted at the time of mastectomy. A 2-stage procedure is when a temporary expander is placed at the time of mastectomy and gradually expanded to stretch the skin. The expander will be exchanged for a permanent implant at a later surgery.

II. Surgery (Axillary Surgery)
Sentinel Lymph Node Biopsy (SLNB)
Sentinel Lymph Node Biopsy (SLNB) is recommended for early-stage breast cancer when the lymph nodes in the armpit do not appear to have cancer.
Sentinel lymph nodes (SLN) are the first few lymph nodes in the armpit where the lymphatic vessels from the breast drain to. These will be removed during surgery and examined under the microscope (frozen section) to determine if cancer has spread to the SLN.
This is done under general anaesthesia (GA). A blue dye or a radioactive substance is injected around the cancer site or at the nipple prior to surgery to locate the SLN. The radioactive substance will be injected before the operation. The blue dye will be injected during the operation.
If cancer is detected in the SLN, lymph nodes in the axilla will be removed. If no cancer is detected in the SLN, no further surgery is needed.
The final histology (microscopic assessment) will be reviewed about 1 week after surgery. In up to 5 percent of cases, the final assessment of the SLN may be different from the initial frozen section result and a second operation may be recommended.
If the dye or radioactive substance is not able to identify the SLN, removal of all the lymph nodes (axillary clearance) will be done.

Axillary Clearance
Axillary Clearance is the removal of all lymph nodes from the underarm when the lymph nodes are found to have cancer cells.
Side effects of axillary clearance include shoulder stiffness and numbness of the inner part of your upper arm. Lymphoedema (swelling of the arm) may occur in 10 to 15 percent of women. This is because lymph nodes drain fluid from the arm and their removal may cause fluid to accumulate in the arm on the operated side.
A separate axillary incision is often needed for patients undergoing breast conserving surgery.
Complications from Surgery
As with all surgical procedures, complications can occur. Risks of general anaesthesia include allergy to anaesthetic agents, heart attack, stroke and deep vein thrombosis, especially for longer surgeries.
Our anaesthetists will assess all patients before surgery to ensure they are optimised and prepared for surgery to minimise these risks.
Surgical complications include:
- Intraoperative injury to blood vessels and nerves in the axilla
- Early post-operative complications of bleeding and wound-healing such as:
- Skin and tissue necrosis and infection
- Seroma formation (accumulation of tissue fluid in wounds)
- Long-term effects of:
- Lymphoedema (swelling of the arm)
- Shoulder stiffness
- Numbness of the breast or chest wall and inner upper arm
Breast Care
After surgery is planned, referral to the Breast Care Nurse (BCN) Service is necessary. Our Breast Specialist Nurse will explain and explore concerns and issues pertaining to breast cancer and the treatment options, and plan pre-operative, operative and post-operative management to ensure successful treatment and recovery.
Consult time for individual patients vary from 30 to 75 minutes. A personal contact number will be provided for convenience and the BCN will be a resource person for patients and their families in the coordination of the various appointments before and after surgery in the treatment journey.
Post-operative services include wound and drain care, rehabilitation, education programmes and prosthesis-fitting.

Radiation Therapy
What is radiation therapy?
Radiation therapy, also called radiotherapy, is a form of local treatment that uses high-energy X-rays to kill cancer cells in a part of the body. It aims to reduce the risk of cancer returning in the area where radiation was given, and together with surgery and other treatments, increases the chance of you staying cancer free. Radiation can be delivered through External Beam Radiotherapy (EBRT) or Intra-Operative Radiotherapy (IORT).

When is radiotherapy done?
Radiotherapy is almost always recommended after breast-conserving surgery and often in patients with high risks disease after mastectomy. This include patients with large tumours and those where the cancer has spread to involve multiple lymph nodes. Almost always, radiotherapy is performed after surgery and chemotherapy, when needed.
How is radiotherapy done?

Radiotherapy is performed over a period of time, which may vary in duration between 1 to 6 weeks. The actual treatment duration will be determined following a consultation with your specialist based on an assessment of your needs.
Following this consultation, an appointment will be made for scans to be performed of the part of the body to be irradiated. This process is called CT-Simulation. During this session, you will meet with our team of Radiation Therapists who will determine the best treatment position for you and obtain a CT scan of the area to be treated.
Your doctor and team of specialists will then perform a personalized planning for radiotherapy according to your needs. Computerized treatment planning is used to optimise the delivery of high radiation dose to the treatment area, while reducing radiation dose to vital organs like your heart and lungs.
Radiotherapy is delivered every day, 5 days a week for the duration of the treatment. Daily treatment lasts between 30 to 60 minutes and is performed on an outpatient basis. Treatment is entirely painless and without any perceptible sensation.
What side effects can I expect?
Radiation affects both cancer and their surrounding normal cells. Cancer cells are typically more sensitive to radiation than normal cells, and are less able to repair themselves after being damaged by X-rays. Hence, they die off after radiation. Even though the surrounding normal cells can be affected by radiation, they often recover with time. This can manifest as side effects that originate from the site of treatment, many of which are short-term and temporary, although there are some cases where long-term complications may also occur.
Early side effects can occur during radiotherapy, typically 2 weeks into the treatment. Such side effects are usually temporary and show gradual improvement in 8 weeks upon completion of treatment. However, some may take a longer time to resolve. Examples of such early side effects include fatigue, skin changes such as redness, pigmentation, dryness and itching, or discomfort from temporary breast swelling.
Late side effects are uncommon and may occur only many months or years after treatment. A small proportion of patients may experience progressive hardening of the breast and the overlying skin which may lead to a shrinking or distortion of the breast or chest wall. Other late complications to the heart and lungs are much rarer and your doctor will advise you further as the risks vary between patients.
Intraoperative Radiotherapy (IORT)
What is intraoperative radiotherapy?
Intraoperative Radiotherapy (IORT) is a specialized form of radiotherapy used in the treatment of breast cancer. Like all radiotherapy, high energy radiation is used to damage and kill cancer cells, so as to reduce the amount of cancer in your body and increases the chance of you staying cancer free.
When is intraoperative radiotherapy done?
IORT is performed only in patients undergoing breast-conserving surgery. Additionally, IORT is suitable only for patients with early stage cancers and meet conditions that your radiation oncologists will advise you on.
How is intraoperative radiotherapy done?
In suitable patients, IORT is performed during the cancer surgery immediately upon removal of the tumour. A specialized applicator will be placed into the excision cavity to irradiate the immediate breast tissue from inside out hence limiting the dose to the rest of the involved breast and normal organs. As patients will remain under anesthesia, IORT is completely painless.
For most patients, this single fraction IORT will be the only radiotherapy they require, hence the treatment burden in well selected patients can be reduced. Occasionally, the surgery and subsequent examination of the cancer may reveal additional information about the cancer which may lead to your doctor recommending for the use of additional external beam RT after IORT.
What side effects can I expect from intraoperative radiotherapy?
Patients will experience the usual symptoms relating to breast cancer surgery. In addition, some patients may experience a slower resolution of the seroma associated with the surgical cavity. A smaller group of patients may find localized hardening of the breast tissue and skin in the region of the operation. Rarely, this may lead to a distortion of the breast in the long term.
SYSTEMIC THERAPY FOR BREAST CANCER
1. Chemotherapy
This treatment uses anti-cancer drugs to prevent cancer cells from growing and reproducing themselves. These drugs are usually given by injection through veins into the blood stream to all parts of the body.
It is usually given over 3 to 6 months and may be used alone, before surgery (neoadjuvant) or after surgery (adjuvant) therapy, or together with targeted therapy to increase the effectiveness of the treatment, depending on the type and stage of cancer.
Chemotherapy is given in cycles. Each cycle consists of a treatment period followed by a resting (recovery) period. As cancer drugs also affect normal cells, the resting period is to allow the body to recover before the next treatment cycle starts.
- Side Effects: There are side effects associated with chemotherapy such as hair loss, nausea and vomiting, loss of appetite, mouth ulcers and risk for infection. However, these are temporary and steps can be taken to prevent or reduce them. Please refer to the chemotherapy educational material provided by your healthcare team for more information.
In some specific cases of triple-negative breast cancer, chemotherapy may be combined with immunotherapy which is a novel type of therapy that is designed to activate the immune system to attack cancer cells. While generally tolerable, they may cause immune-related adverse effects and your oncologist will assess if you are suitable for such treatment.
2. Targeted Therapy
Breast cancers are also tested for special receptors. One such receptor is the Human Epidermal Growth Factor 2 (HER2) receptor. This receptor is over-expressed in about 25 percent of all breast cancers; the presence needs to be confirmed by laboratory tests performed on the biopsy specimen before the treatment is given.
The aim of the treatment is to reduce and hopefully eliminate existing cancer cells in the human body while minimising side effects on normal cells.
Trastuzumab, also known as Herceptin®, targets the HER2 (Human Epidermal Growth Factor 2) receptors on cancer cells to prevent cell growth and division.
Herceptin® has been shown to prolong survival in breast cancer patients with early and advanced disease (Stage IV) when used in combination with chemotherapy.
- Side Effects: Patients who receive trastuzumab may complain of infusion-related reactions such as fever and chills. Rarely, weakening of the heart muscles (also known as cardiomyopathy) has been observed in some patients.
An increasing number of targeted drugs are becoming available for the treatment of breast cancer, including Lapatinib (which targets HER2 and EGFR) and Bevacizumab (which targets a factor associated with new blood vessel formation in tumours.
3. Hormonal Therapy
Breast cancers are tested for oestrogen receptors (ER) and progesterone receptors (PR) on their surfaces as such cancers can be stimulated by oestrogen or progesterone to grow.
Hormonal therapy is aimed at blocking this effect. The drug recommended is dependent on the menopausal status of the women.
Hormonal therapy can cause some side effects, and they are dependent on the type of drug taken and can vary from one patient to another.
- Tamoxifen
This drug blocks the action of oestrogen on the body but does not stop oestrogen from being produced. Tamoxifen may cause hot flashes, depression or mood swings, vaginal discharge or irritation, irregular menstrual periods and sometimes menopause.
Any unusual bleeding should be reported to the doctor. It is recommended for pre-menopausal women, but can be used in postmenopausal women.- Side Effects: Serious side effects from Tamoxifen are rare but Tamoxifen can cause the formation of blood clots in the veins, especially in the legs. In a very small number of women, Tamoxifen can cause cancer in the lining of the uterus.
You may be referred to a gynaecologist to evaluate any unusual bleeding.
- Side Effects: Serious side effects from Tamoxifen are rare but Tamoxifen can cause the formation of blood clots in the veins, especially in the legs. In a very small number of women, Tamoxifen can cause cancer in the lining of the uterus.
- Aromatase lnhibitors (AI)
For post-menopausal women, another group of drugs called aromatase inhibitors (AIs) is also used in breast cancer hormonal treatment. Aromatase inhibitors work by blocking an enzyme called aromatase that the body uses to produce oestrogen.
The current Als such as anastrozole, letrozole and exemastane, are welltolerated and are used in the treatment of early stage and advanced breast cancer.- Side Effects: Side effects of AI include hot flashes, mood changes, nausea, vaginal dryness, joint pain/stiffness, tiredness, lethargy and osteoporosis (including a higher risk of fractures compared to Tamoxifen).
An increasing number of novel therapy agents are becoming available for the treatment of hormone-positive breast cancer in both the early and later stage setting. These can be newer hormonal agents like selective estrogen receptor degrader (SERDs). They can also be targeted therapies that work in conjunction with hormonal therapy mentioned above. These include CDK4/6 inhibitors and PI3K/AKT inhibitors. While generally tolerable, they may cause different side effects to hormonal therapy and should be discussed with your oncologist.
- Side Effects: Side effects of AI include hot flashes, mood changes, nausea, vaginal dryness, joint pain/stiffness, tiredness, lethargy and osteoporosis (including a higher risk of fractures compared to Tamoxifen).
Follow-Up Care
Regular follow up by the doctor after treatment is recommended due to the risk of developing breast cancer again.
This will include physical examination of the chest, underarms, neck, and the other breast with periodic mammograms.
Changes to look out for include:
- Changes in the surgical scar and treated area
- Any unusual changes in the treated or other breast
- Swollen lymph glands
- Bone pain
- Persistent cough
- Difficulty in breathing
- Jaundice
Post-Surgery Care
What is post-operative care for breast cancer like?
Wound and Drain Care
Wounds are often closed with absorbable stitches, hence stitch removal is not needed.
Wound care is simple and patients will be taught and given specific instructions in the management of various types of wound coverage.
Patients are recommended to shower 2 days after most surgeries such as breast-conserving surgery and simple mastectomies.
Soft flexible tube drains are placed under the skin at the time of surgery. These help to remove blood and other fluids that accumulate at the site of surgery. Patients without breast reconstruction surgery are usually discharged from the hospital with the tube drain on the day after surgery.
The nurse in the ward will teach the drain care and provide a chart to keep a record of the drainage, to be reported to the Breast Care Nurse (BCN) daily. The drain will be removed in the clinic when the drainage is minimal and this usually takes 1 to 2 weeks.
Patients are recommended to see a doctor if there is:
- Fever (temperature of 38°C and above)
- Redness/swelling around the opera-tion site
- Discharge from the wound or around the drain site
- Increased pain at the operation site
- Wound breakdown i.e. the skin separates at the wound site
Medication and Diet
Routine medications prescribed by doctors are usually resumed immediately after surgery and there are diet restrictions unless otherwise advised by the doctor.
Activity and Rehabilitation
Patients are encouraged to resume normal mobility and function as soon as it is suitable after surgery.
Most patients with breast-conserving surgery (BCS) and simple mastectomies will be able to resume usual daily activities immediately after surgery, with special precautions for those with breast reconstruction surgery, where management will differ according to their surgeries.
Arm Exercise Programme
Our Arm Exercise Programme conducted by our Occupational Therapists or Physiotherapists on the day after surgery aims to prevent shoulder and arm stiffness. This will enable you to use the arm as you had before surgery in activities at home, work and in recreation.
The exercises also promote circulation of the lymphatic system, thus preventing swelling of the affected arm. Over-strenuous activities are to be avoided in the first few weeks after discharge.
These exercises are to be done once daily, and each set of exercises is to be repeated 5 times. Instructions from the Occupational Therapist or Breast Care Nurse on the limitations will be advised as needed.

Arm and Hand Care
Following axillary surgery, lymphoedema and increased risk of infection of the arm may occur as lymph nodes also contain cells which fight infection.
Therefore, extra care to protect the hand and arm on the operated side from injury is recommended.
Patients will be referred to a physiotherapist or occupational therapist specially-trained in treating lymphoedema. They will recommend programmes which include skin care, exercise, manual lymphatic drainage (a special massage technique), and compression garments to help reduce the swelling.
Preventive measures include:
You will be referred to an occupational or physio therapist for rehabilitation advice and arm exercise. Exercises may begin as early as the first post-operative day. The following basic steps can greatly reduce the risk of arm swelling:
Good skin care is essential in preventing an infection and subsequent swelling
- Use body lotion regularly to keep your skin moisturised.
- Avoid getting an injection or have blood taken from the arm on the operated side, whenever possible.
- Be extra careful to avoid cuts and wounds to your hands and fingernails, especially during activities like sewing, food preparation, gardening and manicure.
- Wear protective gloves prior to contact with chemicals or when immersing your hand in water for prolonged periods.
- Wear long sleeves when outdoors to avoid prolonged direct sunlight. Use sunblock with SPF of at least 30 to protect your skin from sunburn.
- Use insect repellent to prevent insect bites.
Avoid extreme heat on affected arm pathway
- Do not apply hot oil or heat-producing products (e.g. heat rub cream) on the arm, neck and back of the operated side.
- Avoid prolonged exposure to heat e.g. hot springs, saunas and steam baths.
Care for wounds, cuts or burns, and recognizing the symptoms of infection
- Cleanse the area with sterile normal saline or antiseptics. Dry the area and apply a simple, sterile dressing over the wound.
- Observe for symptoms of infection such as redness, swelling, warmth, pain and fever. Consult your GP early, as oral antibiotics may be needed.
Avoid any constrictions to the arm as this might restrict the flow of lymph fluid
On the operated side,
- Do not wear tight jewellery or clothes with tight sleeves.
- Do not hang handbags or shopping bags over your forearm.
- Avoid blood pressure taking.
- Avoid acupuncture.
- If you do go for a deep tissue body massage, request for the masseur not to exert deep pressure.
Maintain exercise to maximize lymph flow
- Use your affected arm, as you would normally do when combing your hair, bathing, dressing, and eating.
- Build up the duration and intensity of exercise or strenuous activity gradually over time.
- Obesity increases the risk of lymphoedema. Reduce weight through exercises and change of dietary habits.
- Continue to exercise your arm after surgery / radiation until you regain normal range of shoulder and arm movements.

Avoid overuse or fatigue of your arm muscles
- Avoid using the arm on the operated side to carry very heavy items, for prolonged periods of time.
- Take more frequent rest breaks when scrubbing, mopping, cleaning, or while doing other vigorous or repetitive activities, especially if your arm feels tired, heavy, or achy.
Physical Appearance
With a mastectomy, physical appearance can be maintained by wearing a prosthesis (called a breast form), or by undergoing breast reconstruction.
There are women who choose not to have breast reconstruction after mastectomy. Some make this decision because they want to avoid extra surgery. For others, it is because they are comfortable with their appearance and body image.
Breast forms or prostheses are used to maintain appearance and a sense of balance, as well as to relieve the strain on posture that may occur after a mastectomy. They are available in a variety of sizes, shapes and colours. Some are designed to fit into a special bra. Others can be attached securely to your chest using a special adhesive.
- Our BCN will give you an appointment for prosthesis-fitting about 6 weeks after the surgery. In the meantime, you may use soft padding underneath your bra while your wound heals.
- When choosing a breast form, it is important that it has the same size and weight as your other breast. This will help maintain your posture and prevent back strain.

Commonly Asked Questions
How common is breast cancer?
More than 29% of all cancers diagnosed in women are breast cancers. Between 2019 and 2023, about 2,787 women were diagnosed to have breast cancer in Singapore each year.
Nine out of 10 women who go to their doctors with breast lumps have a benign disorder, not cancer. Normal changes associated with the menstrual cycle can make breasts feel lumpy.
Can an injury to the breast cause cancer?
An injury to the breast cannot cause cancer. When the body tries to heal the bruise, it can develop scar tissue. This scar tissue can be mistaken as cancer on mammogram. However, symptoms of injury should subside within a month. If you are worried, seek confirmation from your doctor.
Are most breast lumps caused by cancer?
No. Only one lump out of every 10 will be cancerous. This means that 90% of all breast lumps are not cancer. However, the chance of a lump being cancerous increases as you get older. Some women do not have a definite lump, but can feel areas of general ‘lumpiness’ in their breasts. Often, your doctor will be able to reassure you that this is normal but it is important that you ask your doctor to check thoroughly for any change.
Can a benign (non-cancerous) lump turn into cancer?
The chances of cancer developing in a benign lump may be no different than in any other part of the breast. However, it is very important for you to make sure that the lump is non-cancerous in the first place.
If I have a benign breast problem, am I more likely to get breast cancer?
Occasionally, the risk is slightly higher in some women with particular benign breast problems. However, you will need to talk this over with your doctor.
Do benign breast problems come back?
Generally, no. However, a small number of women will develop new benign lumps in the future.
I felt a lump in my breast, but it didn’t show up in the mammogram. Does that mean I don’t have cancer?
A lot of women who find lumps in their breasts get frightened and they go for a mammogram. When nothing shows up, they’re very happy because they assume it’s not cancer. No test is perfect. Ask your doctor to conduct more tests and find out the cause of the lumps. Even though many breast lumps are not cancerous, you should still bring it to your doctor’s attention.
What if the lump turns out to be cancer?
If breast cancer is detected early, it has a better chance of being cured. You will need to discuss the diagnosis and the best treatment options with your treating doctor.
What should I do if my doctor says my breast problem is nothing to worry about but I still feel concerned?
If your doctor has suggested your problem is hormonal, you may wish to wait until after your next period to see if the problem is still there. If it persists or if you are still concerned, you may wish to go back to your doctor or seek a second opinion.
What if there is a history of breast cancer in my family?
Women who have a strong family history of breast cancer, such as a mother and/or sister who developed breast cancer before menopause, may be at increased risk of getting breast cancer. If you are concerned about a family history of breast cancer, talk with your doctor. You may also wish to consult a breast specialist.
Will I still have my menstrual periods after breast cancer treatment?
Treatment with chemotherapy and hormonal therapy may cause changes in your menstrual cycle, resulting in irregular menstruation or early menopause. If you are already reaching menopause, your menstrual periods may not return.
Can I become pregnant when I have breast cancer?
The belief is that changing levels of female hormones during pregnancy could encourage the recurrence of breast cancer. However, there is no data to show that this is so. Some doctors will advise you to wait one or two years after completion of treatment before attempting to conceive. Nevertheless, do discuss with your doctor before planning to conceive.
When is a mastectomy recommended?
Some women do better cosmetically with a mastectomy than with the removal of just the lump, since breast reconstruction is now available using tissue expanders or skin flaps. Your surgeon will be able to advise if you are suitable for breast reconstruction.
The Singapore Cancer Society has a Reach to Recovery Programme that provides physical, cosmetic, post-operative and psychological support. The volunteer is usually a female who has undergone a mastectomy.
Early Detection & Prevention
If I go for mammogram screening regularly, will I be exposed to dangerous levels of radiation?
Radiation exposure from modern mammogram equipment is believed to be safe.
I have a lump in my breast. I am frightened to see the doctor in case it is cancer.
Although your worry is understandable, you should see your family doctor as soon as possible. The great majority of breast lumps are not cancerous.
My mother / aunt died of breast cancer. Am I likely to get breast cancer too?
A small proportion of breast cancer is linked to factors that can be inherited from one generation to the next. Depending upon the number of close relatives affected, you may have a greater chance than a woman who does not have a family history of breast cancer. Most family doctors or hospitals will provide information on breast self-examination and mammogram screenings.
Treatment
I have been diagnosed to have breast cancer. Will I get better?
Many women who have had breast cancer live a normal lifespan. Feel free to discuss your own prognosis with your doctor.
Will I need to undergo mastectomy?
This depends on the size, position and type of your breast cancer as well as the size of your breast.
Does radiotherapy or chemotherapy cause disfigurement and long-term damage?
It is uncommon for women to experience lasting damage from modern radiotherapy techniques. Most chemotherapy side-effects are short-term. Nausea and vomiting are controlled in most patients. Hair loss is still common, and you may require a temporary wig. Your periods may disappear during chemotherapy but may return when you complete chemotherapy. However, for women in their late 30s and 40s, menopause may occur early, perhaps increasing the risk of osteoporosis and heart disease. If a fever occurs while you are on chemotherapy, see your doctor immediately in case antibiotics are needed.
Hormone Therapy for Breast Cancer
Why do I need hormone therapy?
Normal female hormones like oestrogen may promote growth of normal healthy breast tissue, but may also accelerate the growth and recurrence of certain breast cancers. Drugs that slow breast cancer growth by interfering with normal female hormone action are generically called hormone therapy. Some breast cancers need the hormone, oestrogen, to grow. Hormone therapy can prevent your body’s natural hormones from activating growth or spread of cancer cells.
What drug will I be given? What does it do?
The most common drug used for hormone therapy for breast cancer is the oral tablet, tamoxifen, which stops the action of oestrogen.
Will I have any side effects? What can I do about them?
You may experience any of the following common side effects:
- Hot flushes/sweats. Wear a thin layer of clothing to keep cool when hot flushes occur.
- Vaginal irritation. Some women experience vaginal dryness or discharge. Notify your doctor who can recommend a non-oestrogen cream or lubricant.
- Irregular menstrual periods
- Some pre-menopausal women experience irregular periods. Some women may find that once they stop taking tamoxifen, their menstrual cycle becomes regular again.
- Other less common side-effects are depression, mood swings and a slightly increased chance of developing cancer of the uterus and deep vein thrombosis. Regular gynaecological checkups are recommended.
How long will I be on hormonal treatment?
When used to treat early breast cancer, tamoxifen is most often prescribed for 5 years. Patients with advanced disease may take it for varying lengths of time depending on their response to treatment.
Why do some women need hormonal treatment while others do not?
Many breast cancers have ‘receptors’ for oestrogen and progesterone. Receptors are proteins on the surface of the cancer cells to which specific hormones (e.g. oestrogen or progesterone) attach themselves. If the cancer has oestrogen or progesterone receptors, it is likely that hormonal treatment would benefit this group of women.
Prosthesis
What choice of prosthesis (breast forms) do I have?
There is a wide range available. The type of breast form you require will depend on your needs. It should closely simulate the weight and shape of a natural breast and your other breast. If you need advice, speak with your Breast Care Nurse.
Can the prosthesis be washed? How do I take care of it?
Yes, the prosthesis can be washed. Instructions on the care of the prosthesis can be found in the box when you purchase one. You should also place the prosthesis in the box when you are not using it.
Breast Reconstruction
What is a breast reconstruction?
Breast reconstruction is an operation to create a new breast to replace the breast which has been removed. Breast reconstruction does not affect breast cancer survival or treatment. The procedure can be performed at the same time as the mastectomy or at a later date. The breast can be reconstructed using an implant such as silicone, normal saline or tissue from your own body. This procedure requires further discussion with your surgeon.
When can breast reconstruction be done?
There are differing opinions on this. It can be done at the time of mastectomy, some months afterwards or even years later. The timing may depend on the type of breast cancer you have, whether you need further treatment (e.g. chemotherapy), how you feel about the loss of your breast or breasts, your general health, and other concerns such as costs. Talk over these issues with your breast surgeon and plastic surgeon. You may wish to ask for a second opinion if you would like one.
Can I exercise after breast reconstruction?
It will be helpful to stay active and to exercise regularly if you can. Light exercise, such as walking after surgery, can assist in the recovery process. The amount and type of exercise will depend on what you are used to and how well you feel. It is best to discuss your concerns with your doctor.
Do I need to go for regular breast screening after a reconstruction?
It is important to have regular scheduled mammograms on the opposite breast. Breast self examination should continue. Check both the remaining and the reconstructed breast at the same time each month. You will learn what is normal for you since the breast reconstruction. The reconstructed breast will feel different and the other breast may have changed too.
Breastfeeding
After being diagnosed with breast cancer, can I still breastfeed my baby?
You can still breastfeed your baby from the unaffected breast. It is not advisable to breastfeed your baby on the breast that is affected by cancer, as it will not be able to produce adequate milk.
Can I breastfeed after lumpectomy and radiation therapy?
Yes, you can. Lumpectomy is not so extensive that it will affect your breastfeeding capacity, but radiation therapy will. The breast treated with radiation may go through the same changes as the normal one during pregnancy, but it will produce little or no milk. You can, however, breastfeed your baby with the other breast.
Can I breastfeed after mastectomy?
Yes, you can still breastfeed your baby with the other breast. Frequent nursing will be necessary at first so as to build up a good supply of milk.
Will I be able to breastfeed after a biopsy?
Yes. A biopsy will not interfere with your ability to breastfeed. Even if you need a biopsy while you are breastfeeding, you can still continue to breast-feed. However, you will need to discuss this with your doctor.
Arm Exercises
Why do I need to exercise?
You are encouraged to exercise your affected arm soon after your operation to prevent stiffness of the shoulder joint.
When can I start doing arm exercises?
It is normal to feel tired for a few days after an operation. You can start the exercises as soon as you feel strong enough. This can be as early as the first day after your operation. The sooner you start, the faster you regain your shoulder movements.
Contributed by
The information provided is not intended as medical advice. Terms of use. Information provided by SingHealth.
Condition Treated At
Department
Surgery and Surgical Oncology, SGH & NCCS
Department
Oncologic Imaging
Department
Radiation Oncology
Department
Medical Oncology
Department
Breast Centre
Department
NCCS Oncology Clinic @CGH
Department
Breast Surgery
Department
Breast Service
Department
Surgery
Department
KK Breast Centre
Get to know our doctors at SingHealth Hospitals in Singapore.
Get to know our doctors at SingHealth Hospitals in Singapore. here.





















